Immunization vs Vaccination
Table of Contents
Immunization | Vaccination | Inoculation
What is immunization ?
- It is the process by which an individual is protected against a pathogen
- This is done by the agent-specific fortification of an individual’s immune system via
- exposure to an infectious agent (The material is known as an immunogen.) to stimulate an immune reaction.
- supplementing the immunity producing antibodies
- to fortify his or her immune system against that agent.
- Immunization is the same as inoculation and vaccination in that inoculation and vaccination use a viable infecting agent as immunization does.
Origins
-
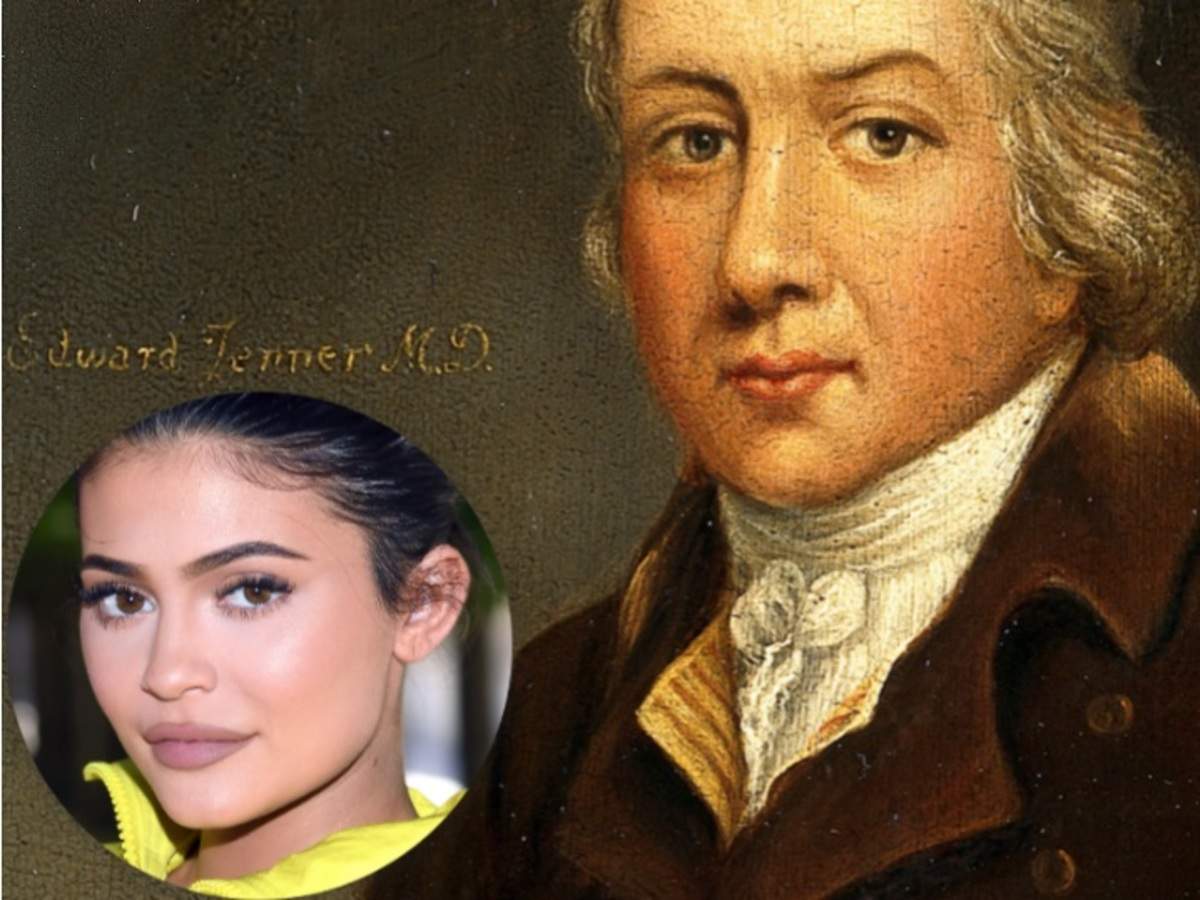
Dr. Edward Jenner (1749–1823) has been widely recognized as the first doctor to undertake sophisticated immunization in 1796. He observed that milkmaids who previously had caught cowpox did not catch smallpox. This prompted him to demonstrate that inoculated vaccinia protected against variola virus inoculation in a 13-year-old boy.
-
Interestingly a British dairy farmer Benjamin Jestey (1736-1816) was the first to notice that “milkmaids” did not ail from smallpox. They instead manifested a milder form of it – cowpox. This inspired Jestey to rather extreme measures, namely, inoculate his wife and children with pus taken from a cowpox infected cows udder. This was found to them immune to smallpox.
.
Definition of a vaccine
Immuno-biological substances designed to produce specific protection against a given disease.
Milestones in vaccination
-
- The term vaccine was coined by – Louis Pasteur
- The term vaccination was coined by – Edward Jenner
- The first vaccine to be developed was against Smallpox
- The first vaccine was developed by Edward Jenner
- The first recombinant vaccine to be cloned in yeast was for Hepatitis B.
Aim of vaccination – Active immunization
- The one-point agenda of any vaccination is to provide lasting immunity against a particular pathogen
- For this, an immunogenic molecule is introduced into a body, which stimulates the body itself to generate immunity
- In contrast, in passive immunization pre-synthesized elements of the immune system (humoral &/or cellular) are transferred into the body which is unable to produce these elements itself.
A Vaccine’s potential for Immune Response
- Usually, a natural infection provides the best possible immune response.
- But a natural infection risks complications and death.
- The ideal vaccine aspires to emulate natural infection in the best potential way without causing the disease or its related complications.
- Hence ideally, a vaccine would be a live organism administered through the pathogen’s natural portal of entry into the host.
- The consequent immune response may be manifested through antibody (humoral immunity) &/or Cell-Mediated Immunity.
- Maternal Cell-Mediated Immunity is not transferred vertically in-utero.
- The goal is to promote a primary immune reaction to enable the organism to exhibit a much stronger secondary immune response on subsequent infection.
- The vaccine emulates the infection with the targeted pathogen, but without the risk of disease causation.
Vaccine Targets
- Every pathogen has a unique antigenic constitution and pathophysiology.
- Vaccines target this uniqueness which varies with the targeted pathogen
- The possible antigenic vaccine targets in a generic infectious pathogen maybe
- Whole-cell – inactivated/killed/attenuated
- Antigenic sub-components
- Proteins
- Carbohydrates (Polysaccharide)
- Toxins
- Endotoxins
- Exotoxins
- Viral or bacterial genetic material
- mRNA
- DNA
Vaccine types
Live attenuated Vaccine
- Attenuated stands for reduced virulence while maintaining antigenicity
- This may be done through serial sub-cultures of the disease-causing pathogen to yield a strain with low virulence.
- In practice, attenuation is achieved by the repeated passage of organisms in tissue culture or chick embryos
- This pathogen of low virulence can be used as a live attenuated vaccine as it is always more potent than a killed vaccine.
Advantages of live attenuated vaccines.
- Live organisms grow and multiply within the host.
- All antigenic components are available.
- Target organs like the GI tract for Oral polio drops may be colonized.
- Live vaccines may multiply and replace wild pathogenic strains prevalent in the community.
Disadvantages of Live Attenuated Vaccines.
- mutations within the attenuated pathogen may turn it into a virulent one resulting in disease causation.
- cannot be used in immunodeficient patients as well as during pregnancy because of fetal risk.
- may require multiple doses, especially in pathogens with multiple strains.
What Precautions need to be undertaken while using Live Attenuated Vaccines?
- More than one live vaccines are usually not administered together.
- They are administered at different sites or temporally spaced 3-4 weeks apart.
- Cholera vaccine and yellow fever vaccine can not be administered together
- Live and killed vaccines can be given together
- Live vaccines are vulnerable to temperature variations requiring specific storage conditions.
- Stabilizing agents are required to be used to ensure potency.
- The freeze-dried formulations are known to enhance the shelf-life of live vaccines before reconstitution.
- Examples.
- Bacterial: Bacillus Calmette–Guerin (BCG) protects against (Milliary and Meningeal Tuberculosis), a typhoid oral vaccine
- Viral: Measles, rubella (MR), oral polio(OPV) (Sabin), Rota Vaccine (Rotavirus), yellow fever, Varicella and Influenza (Flu vaccine)
- Rickettsial: Epidemic typhus
Which pathogen-specific culture strains have been used in vaccine development?
- BCG – Danish 1331 strain
- OPV/IPV – P1,P2 & P3
- Measles – Edmonton Zagreb Strain
- Mumps – Jeryll Lynn Strain
- Rubella – RA 27/3
- Japanese encephalitis – Nakayama strain, SA-14-14-2(Cell culture derived live attenuated)
- Swine flu (Killed) – A7/ California / 2009
- Typhoid -Ty 21 A
- Malaria – SPf 66 (lytic cocktail) & RTS, S/AS01(mosquirix)
- Chickenpox – OKA
- HPV Vaccine
- Bivalent – Cervarix HPV 16 ,18
- Quadrivalent – Gardasil HPV 6,11,16 & 18
- 9 Valent – Gardasil 9 – HPV 6, 11, 16, 18, 31, 33, 45, 52, & 58
- Cholera Vaccine – Dukoral, Sanchol, mORCVAX, orochol
- Influenza vaccine needs re-evaluation every year
Inactivated (Killed) Vaccines
- These are prepared from pathogens killed by treatment with heat or chemicals without denaturing the antigenic component proteins.
- Killed vaccines are comparatively safe but less efficacious as compared to live vaccines.
- They need multiple doses, administered as a sequence of primary doses followed by periodic booster doses.
- The only possibly lethal contraindication is anaphylaxis.
- Examples.
- Bacterial: Typhoid, pertussis(a component of DPT), and cholera
- Viral: IPV(Salk), Rabies(Rabivax & Rabipur) and Japanese encephalitis (JE)
Subunit | Recombinant Vaccines
- The use of the whole organism is associated with a risk of hypersensitivity reaction.
- The antigenic part/sub-unit of the pathogen is preferred to be extracted for the vaccine.
- it is now possible to manufacture the specific antigens utilising recombinant DNA technology.
- In this process, only a part of another bacterium or virus is used to make the pathogen’s antigens instead of using the complete pathogen.
- This helps in excluding the toxigenic parts of the pathogen while including the antigenic components of the pathogen.
- This in turn aids in controlling the side effects of the vaccine.
- The bacterium most commonly employed for this purpose is Escherichia coli.
-Since proteins are more antigenic than carbohydrates, a carrier protein is fixed to polysaccharide antigens to create glycoconjugate vaccines with enhanced immune response. - “Vi polysaccharide typhoid vaccine” uses this technology where only the Vi antigen of typhoid bacillus is used. This vaccine causes fewer side effects, needs a lesser dose and elicits a better immune response.
Toxoids
- The pathophysiology of certain pathogenic bacteria involves endo and exotoxins.
- In such cases, the inactivated toxin (toxoid) is utilised as the immunizing agent.
- Toxoids are usually weak immunizing agents and need adjuvants to enhance the host immune response.
- Adjuvants sensitise the immune system by better antigen presentation (eg. in depot formulation) and/or by giving co-stimulatory signals (immunomodulators)
- Toxoids are produced by the detoxification of toxins.
- The body starts producing antibodies against the toxin on exposure to toxoids.
- They have no inherent protection against infection rather they act against the toxin secreted by the infectious pathogen.
- Toxoids are very safe and highly effective.
- Examples. Diphtheria and tetanus (Component of DPT).
.
Passive Immunization
- Passive immunization is administered using human or animal products.
- Conventionally,
- human products are termed immunoglobulins
- animal products are termed antisera.
- Though animal products are cheaper, they have an enhanced chance of immediate/delayed hypersensitivity reaction.
Human Immunoglobulins
Normal Immunoglobulins
- These provide non-specific, generalized, immediate, ready-made protection for up to 3 weeks.
-One should not be administered any live vaccines for 12 weeks following administration of immunoglobulins. - Ideally, immunoglobulins should be administered two weeks after receiving a live vaccine.
- Examples: Measles and hepatitis A.
Specific Hyperimmune Immunoglobulins
- They protect against specific diseases agents.
- These are developed from the plasma of pathogen-specific recovered patients.
- They are required to be given immediately post-exposure.
- Peak blood levels are achieved in 2 days.
- Specific Hyperimmune Immunoglobulins have a half-life of 3–5 weeks.
- Examples: Tetanus, Hepatitis B immune globulin (HBIG), varicella-zoster immune globulin and rabies immunoglobulin.
Animal Antisera or Antitoxin:
-
- Animal antisera are developed from equine sources.
- The biggest drawback is of potential for anaphylactic reactions and/or serum sickness.
- Examples: Tetanus, Diphtheria, Rabies, botulism, snake bite and gas gangrene.

Leave a Reply