All About Immunization vs vaccination!
Table of Contents

IMMUNITY
Immunity origins
- The word “immunity” is derived from the Latin immunis, meaning exemption from military service or public services
- It is defined as the “ability of an organism to recognize and defend itself against specific pathogens or antigens.”
- Burnet and Medawar, the curious Nobel Prize winners of 1960,
- were recognized for conceptualizing “self” and “non-self,”
- which entailed that the human body had learnt to tolerate its own tissues (as self) but was intolerant to foreign tissues (as not-self).
- Thus, under normal circumstances,
- the body tolerates its own tissues (immunological tolerance)
- recognizes and destroys (“non-self”) foreign tissues.
- In the modern sense, therefore, immunity has been defined as
the ability of the body to recognize, destroy, and eliminate antigenic material foreign to it.
- Immunization has to lead to;
- eradication of smallpox,
- elimination of poliomyelitis
- elimination of neonatal tetanus,
- a marked decrease in the incidence of diseases like
- polio,
- diphtheria,
- pertussis,
- tetanus,
- measles
Infection and its effects.
- The phenomenon of infection may be compared to a home invasion.
- The immune response is akin to the safety precautions undertaken by the legitimate owner.
- The infectious agent originates from infection specific source/reservoir
- It gains access to a susceptible host through its preferred portal of entry.
- The host repels the onslaught through the first line of defence at this juncture utilizing the non-specific Native or Innate Immune mechanisms.
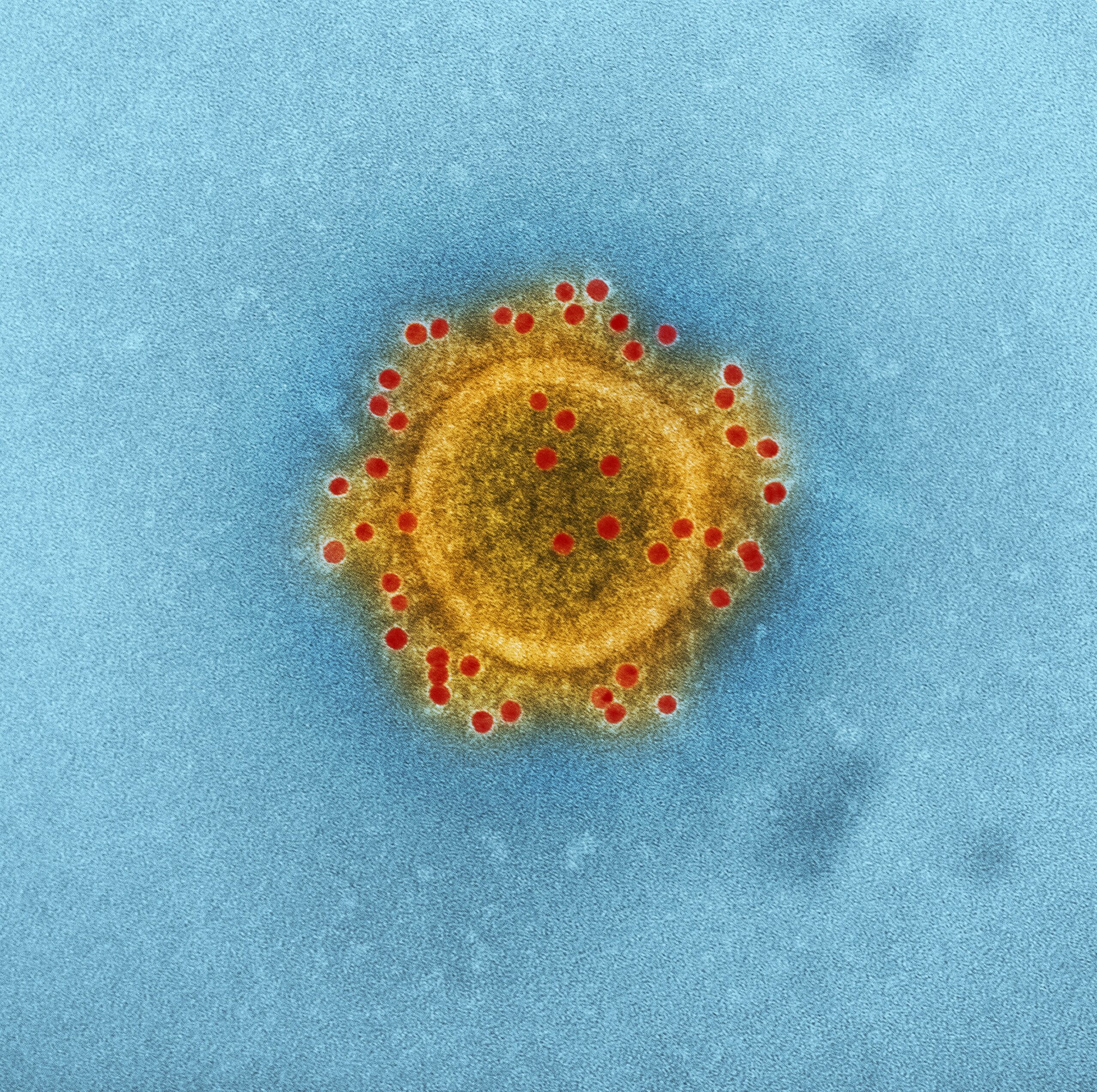
- After penetrating the host’s innate immunity barrier, the infectious agent attaches itself to targeted specific host cell receptors by its surface proteins and gains entry into the host cells.
- This entails a more robust Adaptive pathogen-specific immune response which constitutes the second line of defence.
- The detection of foreign surface proteins on the infectious agent triggers a specific immune response.
- Pathological changes
- cellular lysis due to a multiplication of the agent within the host cell
- toxin-mediated damage to the host cell
- the detrimental effect of the host immune response itself.
Non-Specific | Innate immunity
- These are generic defence mechanisms;
- tears, saliva, gut acidity and other gastrointestinal tract secretions
- They create conditions that neutralize a variety of infectious agents.
-
Similarly at a cellular level non-specific leukocytes, macrophages, as well as chemicals like kinins, are released in a general response to any kind of infectious agent
-
Accordingly, innate immunity is constituted by several sub-strategies.
-
Physical barriers against infection – The skin (integumentary system) and mucous membranes(with superimposed physiological defences created by the ciliary motion of mucus) act as a continuous barrier surface, which must be breached by any pathogen before entering the human body.
-
Physiological limitations such as pH, temperature, and oxygen tension limit microbial growth.
-
Enzymes like lysozyme secreted into external body fluids also resist invasion. Soluble factors within circulation such as complement, interferons, and C-reactive protein are of importance in defence against infection.
-
Phagocytic cells- Macrophages and polymorphonuclear leukocytes (PMN) can recognize bacterial and yeast cell walls through broadly specific receptors (usually for carbohydrate structures), and this recognition is enhanced by complement activation(opsonisation).
-
Specific Immunity
- Characterised by pathogen identification and a specifically targeted response.
- Specific immunity is constituted by humoral components (antibodies) and cellular components (such as T and B lymphocytes)
Active immunity
-
Specific immunity actively mounted and sustained by the host is termed as Active immunity.
- It could be acquired by hosting a particular infectious agent and mounting a specific immune response in due course of nature
- artificially by way of administering vaccines.
Passive immunity
- Immunity passively “gifted” by an external source—termed as Passive immunity.
- It could be acquired naturally via the transfer of maternal antibodies to the child in utero or through breast milk.
- May be acquired artificially by administering immunoglobulins.
Host Defenses
There are two different types of host defences on antigen exposure, classified based on the primary mechanism involved. These are:
- Humoral immune response, which involves activation and clonal selection of B-cells, resulting in the production of antibodies
- Cell-mediated immune response, which involves activation and clonal selection of cytotoxic T-cells
The sequence of events
- The pathogen is engulfed by an antigen-presenting cell (APC) at the portal of entry.
- It undergoes lysis by lysosomal enzymes and the antigens get sieved out
- The antigens are taken up by Major Histocompatibility Complex(MHC) molecules to the cell surface.
- The antigens presented by the APCs activate the T lymphocytes around them.
- The activated T-lymphocytes convert into Cytotoxic T-cell (Tc) & T-helper cells (Th).
- The Th cells sensitize B-Lymphocytes to undergo clonal selection and produce specific antibodies.
- The Cytotoxic T-cell mediate Cell-mediated immune response.
Humoral Immunity
- An activated B-cell specialise into an antibody-secreting Plasma cell and memory B-cell.
- When the host is exposed to a new antigen, the initial immune response also termed as primary immune response takes 7–10 days.
- The primary response is the elevation of pathogen specific-IgM within 7–10 days
- This is followed by a specific-IgG response seen 3–4 weeks after infection.
- The specific antibodies bind to antigens on the pathogen and eliminate them by the way of phagocytosis or complement-mediated mechanism.
- The memory B-cells remain dormant and undergo maturation over 4–6 months.
- During this process, the mutations allow for an increase in the affinity of the specific antibody.
- When the host is exposed to the same antigen for a second time, the memory B-cells are activated within a short duration, i.e., within 24 hours.
- This is termed a secondary immune response.
- The secondary response exhibits the following features:
- Shorter lag time
- Rapid buildup
- The higher overall level of response
- More specific or better “fit” to the invading antigen
- Utilization of IgG instead of the large multipurpose antibody IgM
Active vs passive immunity
- Humoral immunity is active when the organism generates its own antibodies, and passive immunity is active when antibodies are transferred between individuals.
- Similarly, cell-mediated immunity (CMI) is active when the organisms’ own T cells are stimulated and passive when T cells come from another organism.
Cell-Mediated Immunity
- Macrophages engulf antigens and process them internally.
- This sensitizes the T cells to recognize these antigens.
- T cells are primed in the thymus, where they undergo two selection processes.
- The first positive selection process weeds out to only those T cells with the correct set of receptors that can recognize the MHC molecules responsible for self-recognition.
- Then a negative selection process begins whereby T cells that can recognize MHC molecules complexed with foreign peptides are allowed to pass out of the thymus.
- Cytotoxic or killer T cells (CD8+) do their work by releasing lymphotoxins, which cause cell lysis.
- Helper T cells (CD4+) serve as managers, directing the immune response.
Local Immunity
- Local immunity is believed to be produced
- by fixation of various specific humoral antibodies in tissues and cells, or
- it may be a non-specific response of local tissues induced by a local application of antigen,
- against a subsequent infection threatening systemic disease,
- for example, the oral polio vaccine (OPV) is used for producing immunity against poliomyelitis.
Types of Immune Response
- The first encounter with an antigen is known as the primary response.
- Re-encounter with the same antigen causes a secondary response that is more rapid and powerful.
- The immune response depends on the following factors:
- Nature and dose of antigen
- Route of administration
- Type of adjuvants used
- Nutritional status of the recipient
